This resource is for the carers and loved ones of people doing an online program at THIS WAY UP. It offers some answers to commonly asked questions and provides ideas for supporting yourself and your loved one.
There is no ‘one size fits all’- not everyone doing a THIS WAY UP program wants to involve others, but often it can be helpful. Some ideas in this resource may suit you and other ideas may not. Perhaps you and your loved one will read through this resource together and talk about what fits for you.
We’d like to thank Lived Experience Australia, and all the carers and THIS WAY UP users who contributed to this resource – you can read about their experiences in italics throughout this guide. This resource was generously funded by the St Vincent’s Inclusive Health Innovation Fund. To save or print a copy of this resource, click here for the PDF version.
What Is Anxiety and Depression?
Anxiety can be paralysing, and depression can be so deep that you really do need some help to get out of that deep pit.
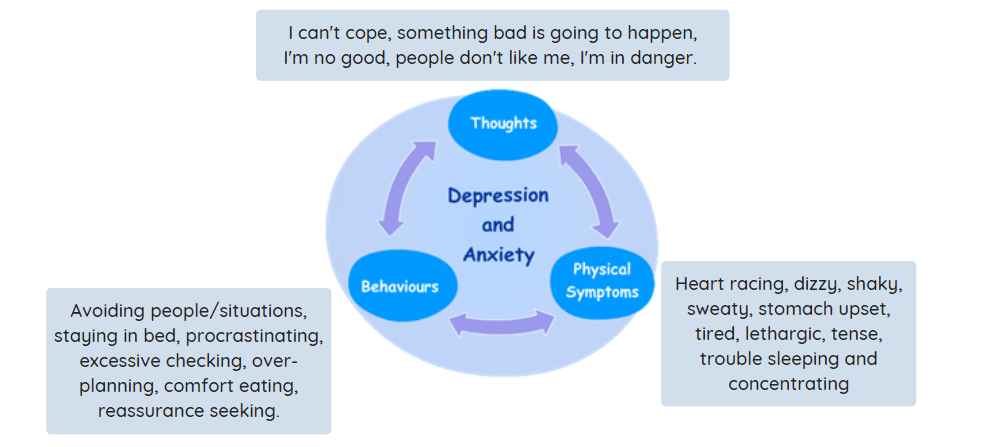
Everyone feels afraid and sad but in clinical anxiety and depression, these feelings are excessive, persistent, and stop the person doing what they want to do. There are three main types of symptoms in anxiety and depression: thoughts, behaviours, and feelings. They interact to keep problems going, and create a ‘vicious cycle’.
In a THIS WAY UP program, your loved one will learn how their own vicious cycle works.
Many people experience stigma around mental health issues, which can be a big source of distress and loneliness. With your loved one, it may be helpful to discuss who to share your experiences with and what information needs to remain private.
I really needed support and people to connect with who understood and know where I am coming from- but lots of people don’t get it. It is hard dealing with other people’s opinions when they don’t know what you are going through. Not everyone needs to know everything- you’ve got to pick and choose.
It is a long term thing for me, lots of ups and downs, lots of stumbles, and that’s ok. Things can change.
What Causes Anxiety and Depression?
Anxiety and depression are very common. We don’t know exactly what causes them but a variety of things can contribute, like genetics, medical conditions, personality factors, trauma, stressful life events, substance use and some medications. Many carers experience feelings of guilt, shame, anger, uncertainty and confusion around this, and often there are no clear causes.
People need to be told over and over again it’s not their fault.
I try to give reasons for why my son is sick, instead of saying just accept that it’s no one’s fault. You want a reason, I want a reason as to why. I still blame myself. I’d love someone to convince me that I can stop that.
Will Things Change?
Yes, symptoms of anxiety and depression often come and go across a person’s life; setbacks are normal and people learn skills to manage their symptoms rather than have them ‘cured’. The changing nature of symptoms can be unsettling, and worries about symptoms getting worse are very common. Progress can take time and may not always be obvious.
These mental disorders are very impactful and the suffering can be quite silent. Change takes time. Just because you may not be seeing progress, doesn’t mean no progress is being made.
It is a long term thing for me, lots of ups and downs, lots of stumbles, and that’s ok. Things can change.
Where Do I Learn More About Anxiety and Depression?
You could read the first lesson or two of your loved one’s THIS WAY UP program or check out the fact sheets at the Royal Australian and New Zealand College of Psychiatrists. Anxiety and depression symptoms can cause a lot of stress for carers and families. It’s common for carers and loved ones to feel a whole range of things like hurt, guilt, grief, fear, resentment, disbelief, sadness, numbness, and exhaustion.
It is frustrating and hard to see him stuck in the same worries and checking over and over again, especially when it affects me and the kids.
I can remember going through stages where I thought, I couldn’t do this anymore. It’s perfectly normal to feel this, it’s ok to be hopeless and helpless.
This is not the job I signed up for. It’s something that’s thrust upon you and more often than not, it’s ongoing.
What Does Treatment Involve?
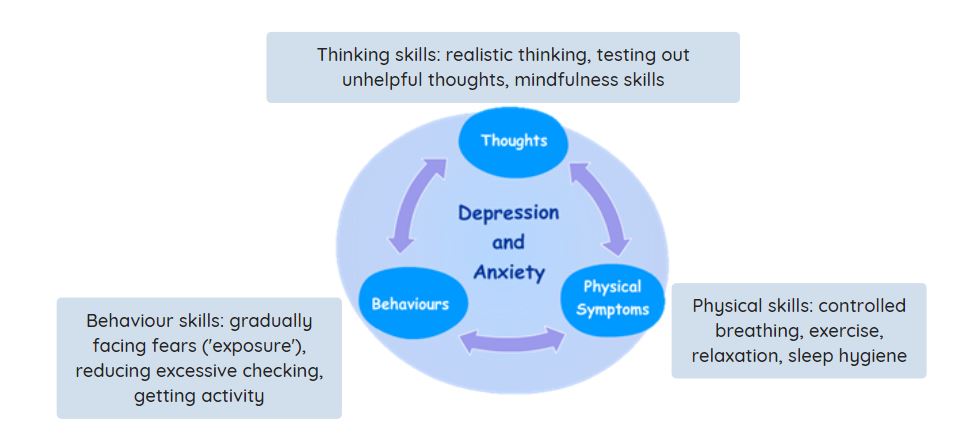
THIS WAY UP programs are based on cognitive behavioural therapy (CBT) which most people benefit from. Individuals have 3 months to do their program and usually spend 1-2 hours each week working on the CBT exercises. CBT breaks the vicious cycle of anxiety/depression by teaching practical coping skills to manage symptoms.
Your loved one may show you their THIS WAY UP lessons and worksheets to help you understand how the skills work, or they may prefer to work through them by themselves.
You may have lots of questions about CBT that your loved one can’t answer. To start, you could take a look at the resources at beyondblue.org.au or make an appointment with your GP or mental health practitioner to ask questions. You may also like to check out one of our free short, wellbeing programs at thiswayup.org.au to better understand what CBT involves. Keep in mind that there can be many other helpful ways of managing anxiety/depression besides CBT (e.g., medications, support groups, other psychotherapies, and healthy lifestyle changes).
It can be very challenging navigating the mental health system, and working out how (or if) you’ll be involved in your loved one’s care. Carers can feel excluded and ‘left in the dark’; not knowing what the plan is or if their loved one is persisting with treatment.
Persevering with the mindless bureaucracy that we’re faced with, that can cause mental anguish and issues in itself. I’ve ticked all the boxes, filled all the forms, but did the person actually get any help? Even though apparently it’s available, practically it’s very difficult to get to.
Where to go to get good consistent treatment is probably the main issue. Clinicians change. They have a good relationship built with a certain clinician and then they just go off after their 6 months, it’s just one of the most horrendous ways our system works. Maybe that’s where NGOs [non-government organisations] come into play, if they’re good NGOs and they have good programs at least they seem to be more consistent with their staff and they seem to stay a bit longer.
My son doesn’t want my help many times- so you have to accept at times that the consumer will not want your help and you have to step away and accept that. And that’s probably one of the toughest ones, particularly if you like to get in and fix things.
Not everyone is ready to get help. You can bring it up over a number of times. You can start the idea one time, then leave it for the next time, and then try again another time- being supportive alongside them over time.
Can I Help My Loved One With Their CBT?
Yes, if they would like you to help. There are lots of ways of helping, but you and your loved one will need to agree on what that will look like for your individual situation. Working out what you are and are not comfortable doing may be tricky and will change over time; it’s a learning process for both of you. When people are struggling, we can rush into problem-solving or ‘fix-it’ mode. This often comes from a place of love and concern, but sometimes one of the best things to do at first is simply listening to their experience.
This is about supporting someone with their self-care management skills. That’s ultimately the goal, to self-manage their illness, to support someone to develop that for themselves.
You’ve got to have permission to be bad at it [supporting your loved one]. It’s not your job to be perfect.
I don’t like to tell the person what to do- rather more like facilitating what they want to do. And identify progress, pointing out those strengths, seeing that it wasn’t so bad after all.
They’ve led themselves really – I learnt to be cheerleading them in the background. You don’t have to feel like you have to nag them or shame them if they’re not doing the program.
It’s not up to me to make [the] other person well, but you can help.

What Practical Things Can I Do To Help?
We have provided a list of things that people often try when supporting their loved one with their THIS WAY UP program, and that may help you generate your own ideas. We would encourage you and your loved one to separately and independently think about the specific things you would like to try before talking about it together.
You may have very different ideas, so it is essential that you and your loved one are comfortable and agree on what will happen. This discussion could be done with a mental health clinician if you prefer, and if you are not comfortable providing the level of support that your loved one is asking for, your loved one could discuss other sources of support and encouragement with their doctor, psychologist or advisory service.
THIS WAY UP Top Tips for Supporting CBT
1. If your loved one finds it encouraging, regularly check in with how they are going, what they are working on with their CBT, and if you can help.
2. Praise and encourage your loved one for their efforts to manage anxiety and/or depression. Focus on the successes, no matter how small they may seem.
3. Help shift your loved one’s attention away from anxious and depressive thoughts and worries by engaging in activities that you both find enjoyable or rewarding.
4. Consider making healthy lifestyle changes with your loved one (e.g., exercise, relaxation, healthy eating, improving sleep, reducing alcohol/caffeine intake).
5. Provide practical assistance to free-up time and energy so your loved one can attend appointments, complete THIS WAY UP lessons, and practice CBT skills (e.g., taking care of children, helping with household duties).
6. If you can, don’t let the anxiety/depression dominate your relationship; have plenty of ‘quality time’ and conversations that have little to do with the anxiety/depression.
7. Get involved with your loved one’s ‘exposure’ exercises if they want the help. Exposure involves gradually and gently facing your fears and doing things you find difficult.
Aim to ‘cheer on’ your loved one rather than give advice or tell them what to do. Offer choices and support if it’s helpful. Your loved one might let you know one or two ‘exposure tasks’ that they want to try each week. You can then support them to ‘stay on track’ and persist when it becomes difficult.
8. Identify the ways you might be unknowingly facilitating or enabling the anxiety/depression.
What does enabling look like?
Doing extra tasks that you wouldn’t normally do (like excessive checking, cleaning, arranging, information-seeking, shopping, calling/texting, accompanying them)
Avoiding situations or activities to avoid the anxiety/depression
Trying to ‘control’ situations to minimise anxiety/depression
Often making excuses, bailing people out, keeping ‘secrets’, covering things up
Doing things for others that would be good for them to do themselves
9. Gently and gradually reduce ‘enabling’ behaviours. Often we do these things because we deeply care about our loved ones, but overtime, it can feel like life starts to revolve around the anxiety/depression. THIS WAY UP programs aim to equip your loved one with the skills to be more independent and confident. Part of this process relies on you slowly reducing these enabling behaviours.
10. As a support person, limit repeatedly reassuring your loved one that their fears are unlikely or are not going to come true. Reassurance can provide relief and comfort in the short term, but this doesn’t last long and prevents your loved one from learning to cope with doubt and distress, and to find out for themselves that their fears are unrealistic.
Develop a plan to reduce providing reassurance and discuss how you can respond when your loved one seeks reassurance. You could let your loved one know how much you care for them and how much you want to help them, but that providing reassurance is not really helpful in the long run. It may also be useful to kindly answer questions with truthful responses like ‘I’m not sure’ or ‘Let’s wait and see’. If your loved one finds the CBT skill of ‘realistic thinking’ helpful, you could also encourage them to ask themselves “what is the evidence that my fears are unlikely to occur?” or “what happened the last time I was worried about this happening?”
How Can I Handle Crisis Situations?
Sometimes anxiety and depression can lead to thoughts of suicide and self-harm. Some people worry that talking about these things will make them happen, but this is not true.
If you would like some practical guidance on having a conversation like this with your loved one, check out the tips at R U OK? (ruok.org.au). It can be very useful to develop a ‘safety plan’ ahead of time with helpful activities and contacts to use in times of crisis and distress (see Beyond Blue safety planning here and the THIS WAY UP Keep Calm, Stay Safe guide here).
Sometimes you and your loved one may need urgent assistance to stay safe. In emergencies, call 000 or attend your local emergency department.
.png)
Taking Care of Yourself
Supporting someone can be challenging. The anxiety/depression may really impact your life and relationships, and at times you may feel overwhelmed, exhausted, isolated, grief-stricken, terrified, or weighted down with guilt or resentment. All these reactions are normal, try to accept your feelings rather than criticise yourself for feeling them.
I didn’t see that I was at rock bottom too, I didn’t have a plan. I had one for my son, but not for me.
When she passed away, it was like I looked up and saw I don’t have any friends and I don’t know what to do with my life… I have dedicated a period of my life, I’ve looked up and thought I don’t know what’s going on now.
It’s hard for me, but you need to have a bit of a life outside of that caring role.
Sometimes you need like a mental walk-away, you know, I’m here for you physically, but I can’t have in-depth conversations about this, let’s park it for now.
Balancing caring for others with caring for your own health and wellbeing is very important. With ‘self-care’ there is no one-size fits all- hobbies, fun activities, good sleep, exercise, relaxation, or just hanging out. Think about what works for you and give yourself time to do it regularly. If you aren’t sure where to start, perhaps speak with your GP and consider the carers’ wellbeing tips and course at Carer Gateway.
Connecting with others who are understanding and supportive is also helpful. This could be with family, friends, and carer support groups, as well as professional counsellors or dedicated carer forums and support lines (see extra resources below). Ideally, relationships are mutually supportive, your loved one with anxiety/depression may also be able to provide support and encouragement in your life.
What if I am Struggling with Anxiety and Depression Too?
Then you are not alone; two thirds of adult Australian carers experience their own significant difficulties with anxiety, depression, and substance misuse. Consider talking to your local GP or psychologist if you are comfortable with that.
Also consider doing your own THIS WAY UP program! There are lots of programs to choose from, and they are all based on good research.
All our programs are free for carers, just send us an email to let us know what program you’d like to do.
Where Can I Get More Information and Help?
Many people find that their local general practitioner or community health centre is a good place to start. More detailed guides for carers can be found from Lived Experience Australia and Beyond Blue.
A variety of organisations provide mental health information and carer resources, telephone support services, and online forums where you can share your experiences and hear from others.


